As virtual health care continues to grow, physicians and patients are utilizing technology to build relationships. We interviewed Dr. Vontrelle Roundtree, MDLIVE’s interim chief medical officer, to share her thoughts about the doctor-patient relationship and how it can thrive with virtual care.

The idea that technology can reduce unnecessary visits to the doctor isn’t new. In fact, when Alexander Graham Bell made history in 1876 by placing the first phone call, he reportedly had a medical issue: He had spilled acid on himself and needed assistance. A mere three years later, well before telephones were common in homes or offices, an article in the Lancet suggested that they could one day be employed to cut down on unnecessary visits to the doctor’s office.
Almost 150 years later, technology has caught up to that early idea with telehealth services such as those offered through MDLIVE, which utilizes video chats and phone calls to connect providers and patients when and where they prefer. (MDLIVE is part of Evernorth, Cigna Corporation’s health services business.)
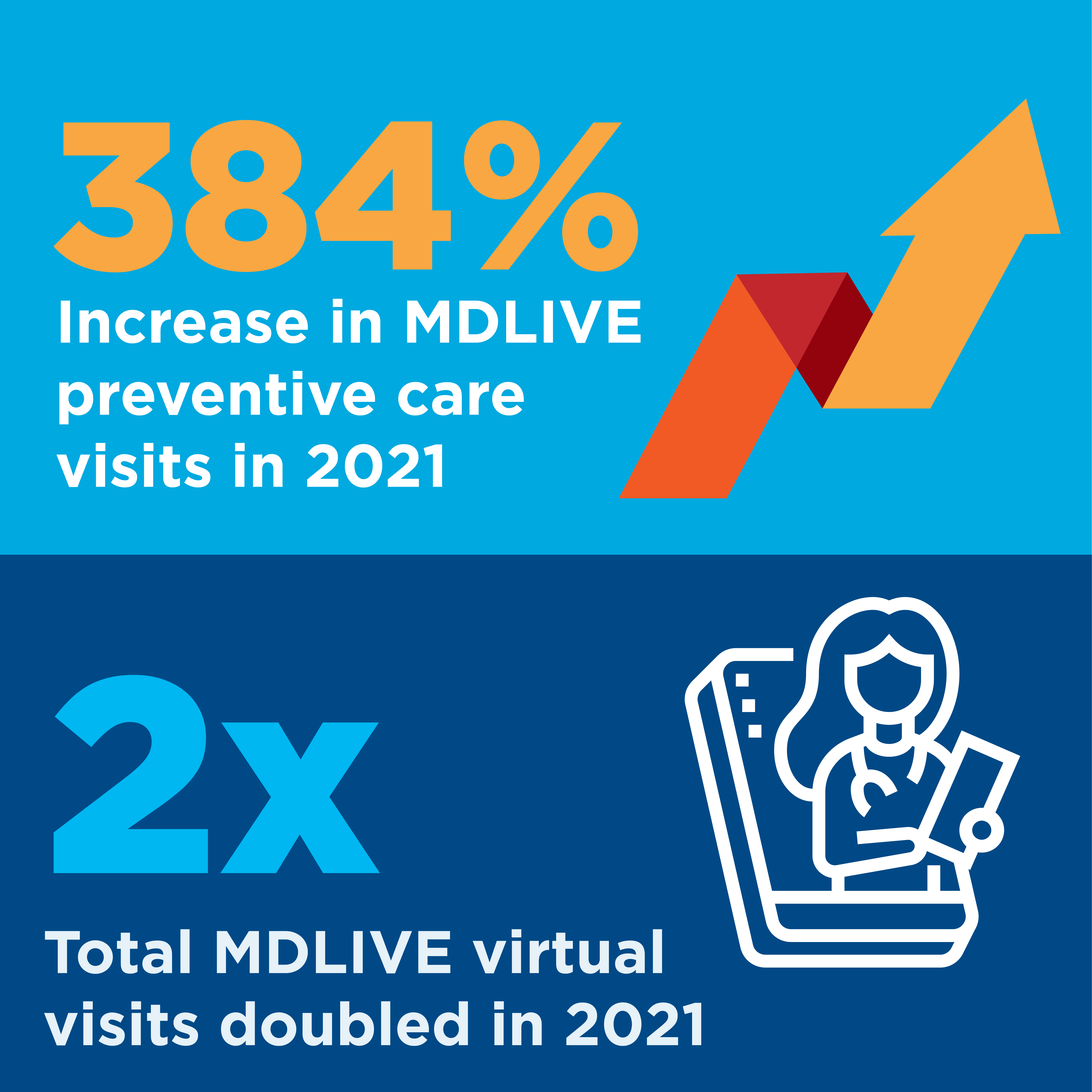 Virtual health care visits soared early in the pandemic, then continued to grow even as offices reopened. For example, MDLIVE saw preventive care visits increase by 384% in 2021 over the previous year, while the total number of virtual visits for primary care services doubled during that time.
Virtual health care visits soared early in the pandemic, then continued to grow even as offices reopened. For example, MDLIVE saw preventive care visits increase by 384% in 2021 over the previous year, while the total number of virtual visits for primary care services doubled during that time.
We asked Dr. Vontrelle Roundtree, MDLIVE’s interim chief medical officer, to share her thoughts about the doctor-patient relationship and how it can thrive with virtual care. Read on for some of the highlights of the conversation.
Tell us about yourself.
I am a board-certified family physician with more than 20 years of experience in the health care industry. I’ve had many opportunities to work in a variety of settings, everything from urgent care to hospice, but I have found great joy and energy practicing family medicine. As a family physician, relationships with patients can span a lifetime, and they become even more important when someone is facing a difficult diagnosis. I find it particularly rewarding to be in a position to inspire and encourage patients during what can be some of the most trying and frightening times in their lives and to celebrate with them when the news is good. Since joining MDLIVE in 2018, my primary focus has been virtual care, and I still see patients.
Can you talk about the benefits of virtual visits for primary and preventive care needs?
MDLIVE’s virtual primary care enables patients to develop ongoing relationships with their providers, who can order labs, conduct annual wellness screenings, and provide follow-up care, including chronic condition management and referrals to specialists when needed. Our platform also provides patients who already have primary care physicians with access to interim primary care services when their doctor isn’t available or when an office visit isn’t convenient or medically necessary.
The use of telehealth for primary care, not just acute needs, is filling a critical need and actively addressing one of the health care industry’s biggest challenges: connecting people with preventive care services that can help identify and address common, chronic health conditions when they are in the early stages so they can be more easily managed or prevented altogether.
 Many barriers to preventive and routine care have to do with issues of convenience, cost, and coverage. MDLIVE is helping to close gaps in care by improving access to primary and preventive care services. Our data shows that 70% of patients who completed a virtual wellness screening with an MDLIVE physician had no primary care visit in the previous 24 months, and fewer than 25% of those patients reported having a local primary care provider. We also found that 68% of that group of patients had at least one chronic disease.
Many barriers to preventive and routine care have to do with issues of convenience, cost, and coverage. MDLIVE is helping to close gaps in care by improving access to primary and preventive care services. Our data shows that 70% of patients who completed a virtual wellness screening with an MDLIVE physician had no primary care visit in the previous 24 months, and fewer than 25% of those patients reported having a local primary care provider. We also found that 68% of that group of patients had at least one chronic disease.
How does a virtual wellness screening work?
Doctors who work in telehealth have enhanced our skills for learning about the patient’s medical history, even when we do an assessment over video. We’ve also learned that patients can give us a wealth of information on their physical health. For example, when someone uses a monitoring device for a chronic condition, such as a patient with diabetes who is monitoring blood-sugar levels, they can share that information. Of course, if we think or even suspect that a patient would benefit from an in-person examination, we make that recommendation.
When patients schedule virtual wellness screenings, we ask them to complete a questionnaire before their appointment that has questions about their medical history, their lifestyle – mainly diet, exercise, sleeping patterns, etc. – and any concerns they have about their health. We also ask about social determinants of health, such as loneliness, whether they have adequate housing and access to nutritious food, and their access to health care. In addition, we work with them to get their lab work done before that first appointment. They can go to a local Quest or LabCorp office, whichever is more convenient. Both the patient and the physicians receive the lab results before they meet, and both find it very beneficial to be able to discuss them during the consultation.
In January 2022, Evernorth rolled out a health monitoring program for patients who utilize virtual care, giving providers and patients better insights into their daily health. The program is designed to improve health outcomes for the millions of Americans living with chronic conditions like diabetes, heart disease, or high blood pressure. For patients who have used MDLIVE virtual primary care, participating providers are able to identify people who could benefit from tracking and reporting their key biometrics such as blood pressure, weight, and glucose levels, which will be reviewed during their visits. MDLIVE plans to expand the program later this year with the integration of digital devices that can transmit patient data automatically to the MDLIVE patient portal.
Can you share a virtual-care success story?
One that immediately comes to mind is a patient seen by Dr. Maggie Williams, who is a director of virtual primary care. The patient was battling lung cancer and undergoing chemotherapy in Washington state, where she lived. At the same time, she was caring for her elderly parents in Idaho, requiring her to travel back and forth several times a week. She was unable to get to regular appointments with her primary care physician due to her chaotic schedule.
To make matters worse, the patient had untreated hypertension, she smoked, and she was overweight. Through MDLIVE’s virtual primary care, Dr. Williams was able to help the patient stop smoking, keep up with refills of her blood thinners and hypertension medications, and refer her to resources in her area for support, as well as address some mental health needs. Today, the patient is doing well.
Where do you see virtual care going, both in the short term and the long term?
The growth we are seeing in services such as primary and preventive care and behavioral health is driving a shift for virtual care from its roots in delivering episodic care for low-acuity conditions to delivering longitudinal, whole-person care. This growth is due, in part, to health plans and sponsors looking for new ways to improve quality of care, outcomes, and patient experience while expanding affordable options for accessing medical and behavioral health care.
While virtual care cannot and should not replace in-person care completely, it will play an integral role in care delivery moving forward. There is growing evidence that the two work better together, and consumers want an integrated model that provides options for both. Offering virtual care options to patients can improve outcomes by offering convenient care to those who might otherwise delay it due to time and other constraints while also improving access for individuals who live in areas where provider availability is a challenge.

Get News, Insights, and Inspiration Right to Your Inbox
Subscribe to our monthly newsletter today.