Cigna’s health services business, Evernorth, has released research that links receiving behavioral outpatient care to lower total health care costs.
The COVID-19 pandemic unleashed a devastating effect on people’s mental health and well-being. The Centers for Disease Control and Prevention (CDC) reports that 40% of adults in the United States struggled with mental health or substance abuse during those first months of the COVID spread.
Add to that the fact that almost half of Americans don’t seek professional help for mental disorders, and it’s easy to see that mental health and well-being has become a crisis in and of itself.
At Cigna, we have long been proponents of whole-person health and are committed to improving health care affordability for those we serve. Cigna’s health services business, Evernorth, has released research that links receiving behavioral outpatient care to lower total health care costs.
Impact of Behavioral Health Treatment on Total Cost of Care
Evernorth's new proprietary data analysis suggests that getting help improves overall health and reduces costs.
Indeed, the study of approximately 275,000 customers found that people diagnosed with a behavioral health condition, such as anxiety, depression, or substance use disorder, who receive outpatient care had lower total health care costs by up to $1,377 per person in the first year after treatment. The savings impact was sustainable, with a two-year cost reduction of up to $3,109 per person.
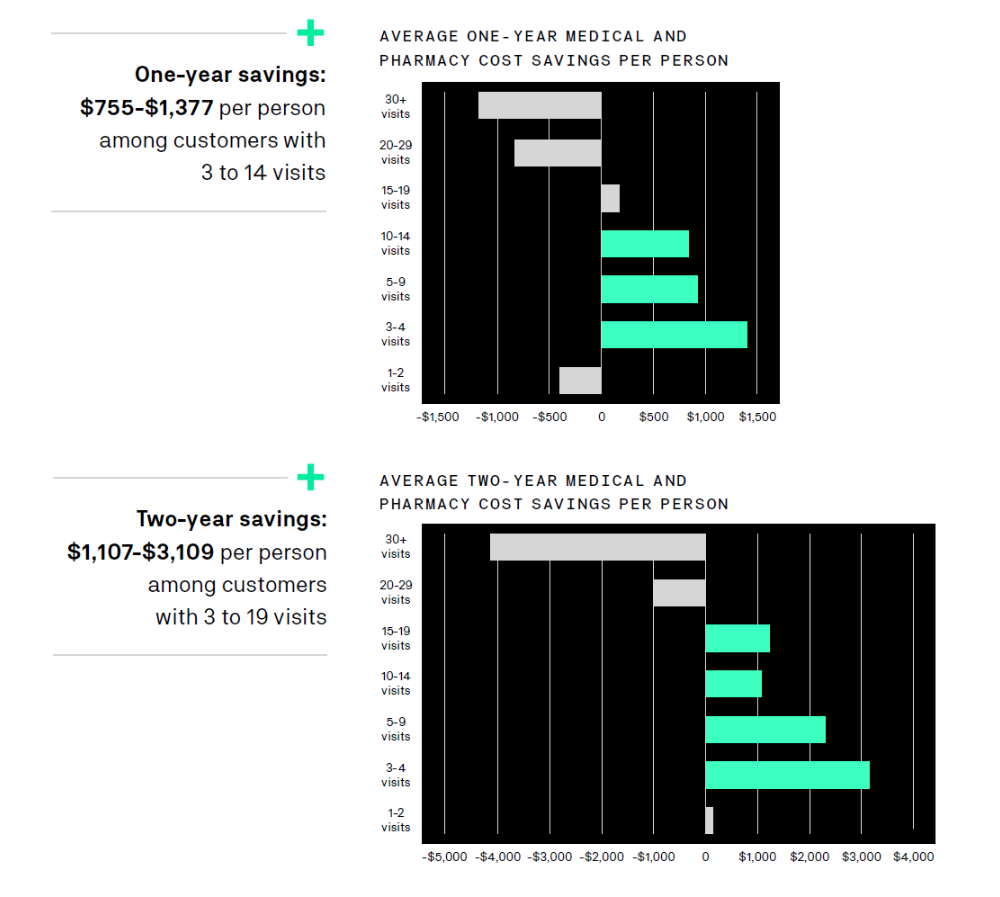
Costs decreased because people utilized fewer medical services, including expensive emergency department visits and inpatient hospital stays. These savings more than offset the costs of behavioral outpatient care and indicate that even the lowest level of treatment can have a significant impact by helping people feel better, mitigating health care costs, and driving improved system-wide affordability.
We sat down with behavioral health professionals and case managers who work directly with customers to better understand the importance and impact of behavioral outpatient care.
What is Behavioral Outpatient Care?
Behavioral outpatient care isn’t one specific type of treatment – it can involve a wide range of different options that can take place in individual or group settings and doesn’t require an overnight stay. It can include help from therapists, peer support groups, or health care professionals who can prescribe medication. With the rise of virtual care, outpatient care can be also accessed from the comfort of one’s home.
“Outpatient care is where the magic happens,” said Jamie Barten, crisis 24/7 triage care manager at Evernorth and a licensed marriage and family therapist. “Outpatient care allows a person to explore behaviors and symptoms that lead to mental health distress, so they can enact new patterns and learn adaptive coping skills over time.
“I often help customers think of behavioral care as a staircase – the ground level built upon outpatient care,” she added. “It can range from entry-level steps like counseling with a therapist once or twice a week to more intermediate steps with more intensive outpatient programming – such as a structured group facilitated by a therapist held multiple times per week.”
Care managers at Evernorth help customers navigate the various levels of behavioral care and screen for risk factors to help determine appropriate next steps for their behavioral care journey.
Unfortunately, many people don’t receive the behavioral care they need, and they often wait until symptoms or behaviors build up and turn into a crisis, Barten said. “Often, when someone is in crisis and I speak with them, they can be in acute distress and require my help referring them to a higher level of care before they are ready to take on outpatient therapy – which could include intensive outpatient programming, partial-hospitalization programing, or inpatient care.”
Overcoming Barriers and Stigma; Building Connections and Trust
There can be a devastating stigma around asking for help, especially when it comes to mental health. One report found that almost half of adults with a diagnosable mental disorder or with a self-reported mental health condition had seen a mental health provider in the previous year. Continued management of mental health is often misunderstood by individuals and society at large.
“Often, people think of behavioral or mental illness as a condition like a tumor – where you can work to get it removed and then try to carry on with your life, which isn’t accurate or helpful,” Barten said. “It’s more analogous to a chronic condition like diabetes, which can be really well managed over the long term.
“With common conditions like depression or anxiety, you can have well-managed years where you are seeing a therapist and taking the appropriate medications. You may even get off medications if you’ve overcome a particularly difficult period.”
Unfortunately, few people see mental conditions in this way, she said, adding that people expect recovery to be instantaneous. Matthew DiStefano, a behavioral social worker at Evernorth and a licensed professional counselor, said that the stigma of being treated for a mental health condition is greater than going to a doctor’s office because of a physical ailment. On the flip side, once people get the help they need, it’s like a lightbulb goes off.
“The thing I hear the most is, ‘I wish I would have done this sooner,’” DiStefano said. “With the help of outpatient care, we see many people transition into a much healthier and productive lifestyle as they start to address their mental health challenges and learn coping skills.”
Another common barrier is access and availability of care, and COVID-19 has reshaped the landscape. At the onset of the pandemic, significantly higher demand for behavioral health services led to difficulty getting an appointment with a therapist. Today, however, COVID-19 has ushered in a new age of virtual care, which has helped provide access with ease and convenience. Before the pandemic, virtual visits made up just over 1% of all medical and behavioral professional office visits that could be conducted virtually. Today, they account for nearly 25% of visits.
With teams of professionals like Barten and DiStefano, Evernorth is uniquely poised to help break through barriers and create the time and space to listen to people’s stories, build connections, and navigate resources.
The Connection Between Physical and Mental Health
Evernorth’s research findings are particularly relevant for people living with co-occurring mental and physical health conditions – such as those experiencing depression alongside diabetes, heart disease, or cancer.
Previous industry research has shown that health care costs for this population can be two to six times greater than for those without a behavioral health condition. Behavioral conditions can exacerbate physical symptoms as well as hamper medical treatment and recovery. That means addressing behavioral health issues for people with medical conditions offers significant potential for cost savings by driving better compliance to medical treatment and improved overall health outcomes.
“In my experience, we see a lot of people who are referred to behavioral resources when seeking treatment for a physical issue,” DiStefano said. “They are intertwined and go hand-in-hand – if you’re not feeling well emotionally, your physical health will suffer and vice-versa. When we treat physical and mental health in tandem, that’s when we are most likely to see the best overall outcomes.”
Working With Employers and Organizations To Increase Awareness, Implement Mental Health Resources
At Cigna, we believe that employers and organizations play an important role in fostering healthy workforces – from the standpoint of physical health and mental health and well-being.
In addition to working with individuals, Cigna works closely with employers and organizations to find behavioral care solutions that fit their unique challenges and to educate them on the importance of mental health.
We spoke with Jason Youngblood, director of Cigna’s Behavioral Center of Excellence (BCoE) and a licensed professional counselor. The BCoE was launched in July 2018 as an innovation lab of sorts, with the aim of enabling Cigna teams to address the challenges our customers and our employees face.
The BCoE team, which serves as a consultant to business leaders across Cigna as well as our commercial business clients, takes a data-driven approach to innovation in the behavioral care space, rapidly moving new services to the market that meet the needs of today’s health care consumers.
“One of unique things about Cigna is that we have both a clinical team aligned to supporting individuals, and we have an organized group supporting organizations,” Youngblood said. “I’m a therapist, but I don’t see individuals. I see and help organizations to improve their behavioral health and well-being.”
Youngblood’s team of licensed clinicians are out in the marketplace every day, helping human resources and benefits leaders navigate behavioral challenges at the organizational level.
“When I started in this specific role around 10 years ago, organizations had a very passive interest in behavioral care,” Youngblood said. “Over the years, we’ve seen a societal shift – organizations are increasingly aware of behavioral issues affecting their employees, but they don’t always have the language to talk about it or the tools to address them.
“We go into an organization that has identified a behavioral health care challenge – maybe they’ve seen increased levels of depression or anxiety, absenteeism, and they’re asking for help. The tools in our toolkit could include basic education, rolling out an Employee Assistance Program promotional campaign, training for managers, as well as onsite resilience coaching – we identify strategies to enable organizations to address their specific challenges.”
Overall, for individuals and organizations, there is a tremendous opportunity to connect more people to mental health support earlier and more often. Those connections, in turn, will lead to better overall health and well-being.

Evernorth Behavioral Health
Evernorth’s data-informed approach to behavioral health provides personalized and customized care across the entire continuum for the populations we serve. These solutions predict emerging health needs, close gaps in care, and drive cost savings—all while empowering whole-person and whole family health.