One of the most frustrating product shortages over the past few months has been at-home COVID-19 tests. As omicron has soared, the tests’ availability seems to have plummeted. That’s beginning to change, however.
Recently, the United States government made available four free at-home COVID-19 tests to each home address upon request. In addition, health insurers now provide or reimburse the cost of up to eight home tests per month for most members. (Cigna members can request reimbursement for tests or get more information at cigna.com/coronavirus.)
The program providing up to eight tests a month originally applied only to those covered by commercial insurance. On February 3, the government announced that Medicare recipients also would gain access to at-home tests at no cost, beginning in early spring. Recipients also continue to have access to free at-home tests from community health centers and Medicare-certified health clinics.
In addition to questions on accessing tests, the accuracy of home tests is often questioned – along with how to select the best tests, how to use them, and when to use them. We asked Dr. Steve Miller, Cigna clinical advisor, for answers to questions about testing and more.
What’s the best, most accurate home COVID test? How do I select a home COVID test?
All at-home COVID tests authorized by the Food and Drug Administration (FDA) are effective. It’s important to remember that they are diagnostic tools that aim to tell you if you are currently infected, but they’re not designed to show if you’ve previously been infected or were infected quite recently and there’s too little virus present in your body for the test to detect.
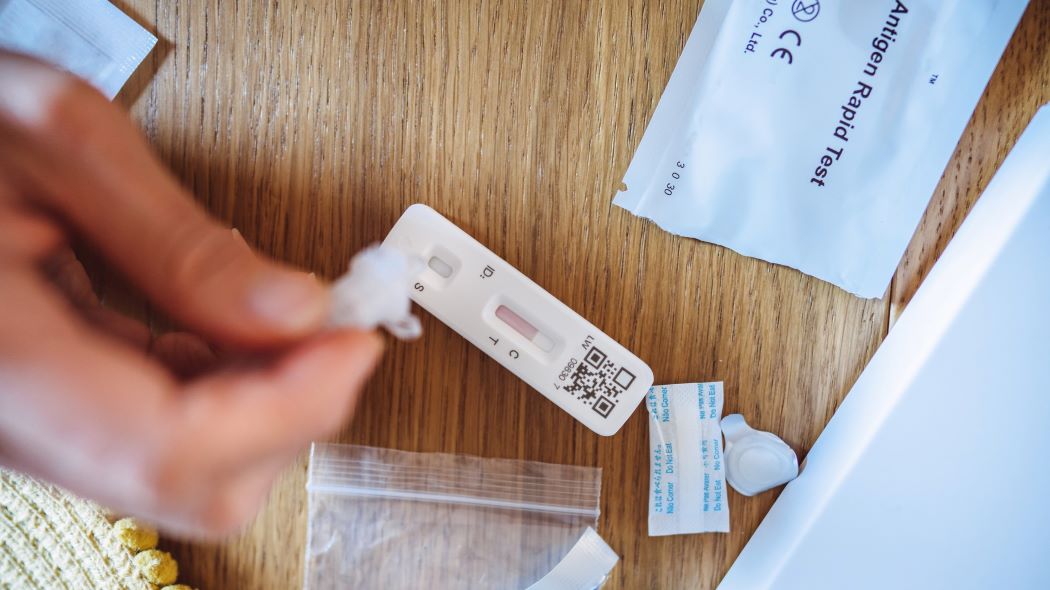
Most home tests are antigen tests. They utilize a nasal or throat swab to identify antigens, which are proteins from the virus. With antigen tests, false positives are rare but can happen – and many brands include two tests per box and are meant to be used within a few days of each other to confirm results.
Can at-home COVID tests detect omicron?
Yes. A recently published study that compared PCR tests to at-home testing found that people infected by the omicron variant and who had high viral loads tested positive.
How do I avoid buying – or inadvertently using – recalled COVID tests?
Most recently, specific lots of the Ellume COVID-19 Home Test were recalled by the FDA due to higher than average risks of false positives. These tests were recalled in mid-December and have been removed from store shelves – a contributing factor to the shortage of at-home tests. If you purchased a recalled test, check the manufacturer’s website to request a replacement.
How do I use a home COVID test? Can I use the same COVID tests for adults and children?
The FDA has authorized some at-home tests for children as young as 2 years old. Check the fine print on the box to be sure it can be used for your child. If you have questions, call your pediatrician or doctor for advice. If you don’t have a doctor, contact your local health department. They can direct you to the best place for testing/treatment.
If my COVID test is positive, what should I do next?
The CDC's Respiratory Virus Guidance recommends that people stay home and away from others until at least 24 hours after both their symptoms are getting better overall, and they have not had a fever (and are not using fever-reducing medication). If you have rapid tests, you can use them to see if you’re still positive and if you need to continue isolating.
Should we worry about false positives from home tests? What about false negatives?
There’s no need to worry about false positives and false negatives, but there is a small possibility. It’s important to remember that any test is a snapshot of what’s happening in the part of your body that was sampled at that moment – that’s all it can report.
False positives are possible but fairly unlikely with antigen tests if the test is taken correctly, especially if you develop symptoms and know you’ve been exposed. If you believe you have a false positive on a home test, it’s worth confirming with a PCR or a follow-up home test.
There can be false negatives with home tests – and with PCR tests – especially if the test is given too soon after the initial exposure (when not enough virus is present in your body), or if the virus is replicating somewhere other than where you swab (such as your throat instead of your nose). This is why it’s important to test again in the next few days to confirm, especially if you develop symptoms.
When should I use a home COVID test? How long after exposure should someone wait to test for COVID?
The question is really which test you have access to first – PCR vs. at-home tests. If you’ve been exposed, you should test within a few days, especially if you develop symptoms.
The CDC recommends testing when symptoms develop. If no symptoms develop, the agency recommends testing five to seven days after exposure. There have been anecdotal reports that people infected with omicron are getting negative results during the initial days of their symptoms. Because of that, it may be good to wait a few days before testing, especially if you have a limited supply of home tests.
Should COVID tests be repeated to ensure accuracy?
Yes. You should test at least twice over the course of a few days. If you have a limited supply of home tests, aim for the times you are most likely to get an accurate result (days five and seven after exposure).
How long in advance should I test for COVID before a social event such as a birthday party?
If you’re totally asymptomatic, test within 24 hours before you arrive at the event. If you have any symptoms, no matter how minor, test and do not attend the event, no matter the results of the test.
How long before getting on an airplane should I test for COVID?
If you’re traveling internationally, follow the guidelines for the country of entry. These guidelines are subject to change, so make sure the guidance you’re following is up to date. Currently, the United States requires a negative PCR test no more than one calendar day before entering the country. Other countries require a negative test that was done 48 or 72 hours in advance.
If you’re traveling domestically, use the same guidance as when you’re planning to attend an event: If you’re totally asymptomatic, test within 24 hours before your trip. If you have any symptoms, no matter how minor, test and do not get on a plane, whether you test positive or negative.

COVID-19 and Kids: Parents’ Most Frequently Asked Questions Answered
As the COVID-19 pandemic continues to evolve, parents might feel like they’re scrambling to keep up with the best ways to safeguard their children. We asked Dr. Steve Miller, Cigna clinical advisor, for his latest guidance based on parents’ most common questions.