
All businesses today – large and small, irrespective of industry – are in the business of healthcare. Forbes has gone so far as to say that the future of work is employee health and well-being.
And rightfully so. In the United States, today’s workforce is grappling with a mental health crisis and rising costs of living while dealing with a tripledemic of COVID-19, flu, and respiratory syncytial virus (RSV) that is keeping many people away from work, driving medical costs, and straining hospitals. Meeting employees’ needs across a plethora of different dimensions that make up their health and well-being has never been more challenging – or rewarding.
Despite those factors, the healthcare outlook for early 2023 and beyond has a number of encouraging trends for the employers who provide health insurance to employees and their families. Read on to learn more about four top healthcare topics and how they will impact American businesses.
1. Heightened Focus on the Vitality and Well-Being of Employees
The body and mind are intrinsically connected, but the complexities of health and wellness go beyond just physical and mental health.
“In 2023, we’ll see a heightened focus on a more holistic approach to health and well-being,” said Dr. David Brailer, chief health officer, Cigna Corporation. “Companies will look beyond just physical and mental health to build wellness strategies that hit on all of the dimensions of people’s lives that impact their health and well-being.”
Cigna has long supported an approach to employee well-being that empowers individuals to attain wellness in each dimension of their lives, particularly when it comes to benefits. We recently partnered with Dr. Richard Ryan to launch the Evernorth Vitality Index, a tool to measure health and wellness for personal, business, and community impact.
Using the Index, we surveyed 10,000 U.S. adults to better understand the state of vitality among the general population as well as the American workforce, and we found that higher vitality – the capacity to pursue life with health, strength, and energy – is linked to a more motivated, connected, and productive workforce. Furthermore, employees with high levels of vitality are healthier, more confident in their jobs, feel supported at work, and are more motivated and productive than those with lower vitality levels. Crucially, those with higher vitality are more likely to stay with their current employer – an important asset for employers navigating the Great Resignation.
Research finds that employer-sponsored wellness programs will yield a 47% average return on investment (ROI) to employers this year. In layman’s terms: For every dollar an employer spends on workforce health, they get back $1.47 in financial benefits.
Employers can support workforce vitality by building a culture of health reflected in all policies, procedures, behaviors, and expectations. This includes taking a holistic approach to benefits, which empowers individuals to attain wellness in each dimension of their lives: financial, physical, emotional, social, intellectual, environmental, spiritual, and occupational.
2. A Strategic Effort To Keep Drugs Affordable
Prescription drugs are the second biggest healthcare expense for employers today, representing about a third of total healthcare costs for businesses. While generic medications account for 90% of all prescriptions, specialty products are at the other end of the affordability spectrum. With an average annual price of $38,000 per patient, specialty medications are used by less than 2% of the population yet account for more than half of overall drug spending in the United States. Biologics – which are derived from components of living organisms such as blood, cells, tissues, or recombinant proteins – can cost as much as $50,000 for a single dose [PDF], and treating one patient can cost hundreds of thousands of dollars per year.
Help is on the horizon. In the U.S., more than 90 biosimilars – clinically equivalent products to U.S. Food and Drug Administration (FDA) approved biologics – are in development today. More than 20 are available for use, with additional biosimilars coming soon.
“Biosimilars hold tremendous promise to improve the affordability of life-changing specialty medications, and this is part of our work to expand access to them and achieve lower costs for the employers and members we serve,” said Katy Wong, chief pharmacy officer, Cigna Pharmacy.
In 2023, we expect to see a number of biosimilar products that can be dispensed interchangeably with Humira, a widely used biologic that treats conditions including rheumatoid arthritis, Crohn’s disease, and psoriasis, reach the U.S. market in 2023. Cigna Pharmacy, which manages pharmacy benefits, will add biosimilars as preferred products on its commercial formularies at the same position as Humira. Pharmacy benefit manager Express Scripts, which is part of Evernorth (Cigna Corporation’s health services division), is also adding inflammatory conditions biosimilars to its largest formularies. Adding biosimilars to these formularies can generate competition, helping lower costs for plan sponsors and patients.
Other relatively new products promise a cure in one dose – at a price that can soar into millions of dollars. In November, the FDA-approved Hemgenix, a gene therapy for people with a rare type of hemophilia. The list price: $3.5 million.
Payers are looking for ways to help plan sponsors and patients afford these important new therapies. For example, Cigna offers Embarc Benefit Protection. Under this program, clients pay a flat per-member, per-month charge, which protects them from the price shock of high-priced medicines such as gene therapies. Patients pay nothing out of pocket and receive personalized, expert care to assist them through their health journey.
3. Digital and Virtual Health Is Here To Stay
As people stayed home to stay safe in the early months of the pandemic, virtual visits with medical offices, behavioral therapists, and even typically hands-on practitioners such as physical therapists boomed. According to the American Medical Association (AMA), 14% of physicians were available for virtual visits in 2016; that number jumped to 80% in 2022.
Interest has grown along with availability. “According to Cigna’s research, availability and access to virtual health has become increasingly important,” said Katya Andresen, Cigna’s chief digital and analytics officer, citing a study that shows 76% of people are interested in using telehealth, compared with just 11% who used telehealth in 2019. Even after the pandemic ends, 83% of patients expect to use virtual care. Sixty percent of consumers’ most recent mental health visits were via telehealth.
In addition to communicating one-on-one using internet conferencing tools, mobile apps, and phone calls, digital health tools provide another layer of care. In 2016, just 12% of doctors were able to utilize wireless remote monitoring devices; today, that number is 30% and growing, according to the AMA study. For example, remote monitoring devices can keep physicians appraised of a patient’s blood glucose levels, heart rhythm changes, and other vital signs. In the future, doctors expect to use devices that can monitor conditions such as epilepsy and chronic obstructive pulmonary disease.
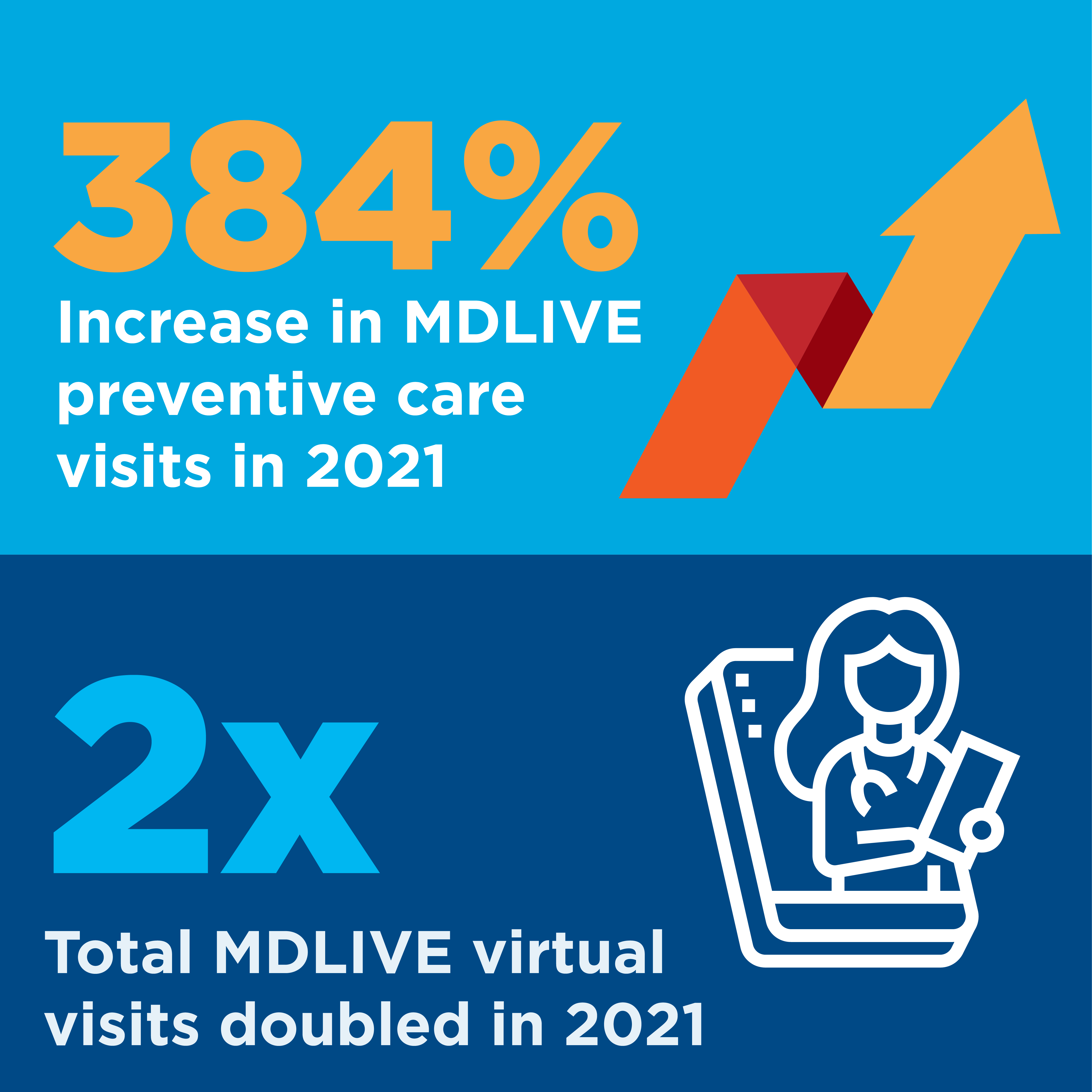 Patients with chronic conditions also are finding value in virtual care. For example, MDLIVE, Evernorth's virtual care platform, is evolving its virtual primary care program to enhance support for patients with chronic conditions. Patients will work with their primary care doctor to develop a care plan that includes condition management and lifestyle goals, lab tests, medication management, and referrals to other health providers. Their care team will track their progress with remote monitoring through connected devices, such as blood pressure cuffs and blood glucose monitoring devices.
Patients with chronic conditions also are finding value in virtual care. For example, MDLIVE, Evernorth's virtual care platform, is evolving its virtual primary care program to enhance support for patients with chronic conditions. Patients will work with their primary care doctor to develop a care plan that includes condition management and lifestyle goals, lab tests, medication management, and referrals to other health providers. Their care team will track their progress with remote monitoring through connected devices, such as blood pressure cuffs and blood glucose monitoring devices.
Just as patients can benefit from readily available virtual care, so can their employers. With the right virtual care solutions, organizations can enjoy better population health, greater employee engagement, increased productivity, and lower total costs of care.
“Digital technology is the key to transforming our fragmented healthcare system and reorienting it around consumers,” Andresen said. “Digital innovation allows us to shape people’s care based on their own unique needs, bringing care into their homes and to their fingertips, and it connects their care across sites and experiences. In 2023, expect to see acceleration of digital adoption and transformation at an unprecedented pace – because adoption is high and the benefits are higher still.”
4. Working To Fix Our Fragmented Healthcare System
Healthcare is complex. In the United States, it’s all too often fragmented. An individual may see numerous healthcare professionals, who rarely have complete insight into the patient’s medical history, prescription medications, and other factors that can – and often should – influence care decisions. That’s why most visits to a new practitioner start with an extensive medical history, requiring dedicated staff time and relying on the memory of the person being seen.
For example, one of the biggest issues in the behavioral health space is the lack of connection to medical and pharmacy care, said Eva Borden, president of behavioral health at Evernorth. She predicts that health tech start-ups will play a role in forging connections that will be crucial to providing whole-person, holistic health care.
"Our clients and customers are exhausted by the fragmented healthcare system,” said Heather Dlugolenski, senior vice president, U.S. solutions, Cigna. “They want one place to go to get a personalized experience for their entire healthcare journey." To address that, we recently announced Cigna Pathwell, a concierge service that creates a personalized end-to-end health journey for patients with complex conditions.
Solutions like Pathwell will help employers by streamlining benefits management, reducing complexity and associated costs while optimizing care for their employees – and healthier employees mean a healthier business.

Related: Address Employee Burnout
Learn how to help your employees improve their vitality—at work, at home, and in their communities—to create a culture of health.